TO: Employees and Retirees Eligible for Benefits under the Fresno Unified School District’s Employee Health Care Plan
DATE: March 16, 2018
In February 2018, the Joint Health Management Board (JHMB) formally initiated changes to Medical Plan Option A (Anthem Blue Cross) and Medical Plan Option C (Kaiser Permanente®), as a result of the labor agreement ratified by the District and Fresno Teachers Association (FTA). To ensure that plan participants are able to make changes to their medical coverage by the June 1, 2018 effective date, the JHMB is offering a Special Benefits Enrollment from April 2 to May 4.
ONLY Medical Plan Changes Allowed During This Special Benefits Enrollment
Please review the following brief highlights in this letter to understand the upcoming changes to Medical Plan Options A and C, and decide if you should make a change to your coverage. If you wish to change your medical coverage (only), you must complete the Special Enrollment Form and return it to the District Benefits Office no later than May 4, 2018. All changes will be effective June 1, 2018.
NOTE: If you do not wish to change your medical coverage for the remainder of the 2018 calendar year, no action is required on your part during this Special Enrollment period. However, if you wish to change your medical coverage, you must complete the Special Benefits Enrollment form.
Changes NOT Allowed During This Special Benefits Enrollment
During this Special Benefits Enrollment, you may only elect to change your medical plan option (i.e. move you and all of your dependents from one plan option to another plan option). However, the following changes are not permitted during this Special Benefits Enrollment period, unless they are due to a family status change:
- Changes to Dental or Vision Coverage
- Changes to Medicare Prescription Drug Plan
- Add/Remove Dependents (except due to a family status change)
- Add/Remove Coverage in the Kaiser Senior Advantage Plan (except due to a family status change)
Please contact the District Benefits Office if you require changes to your coverage due to a family status change.
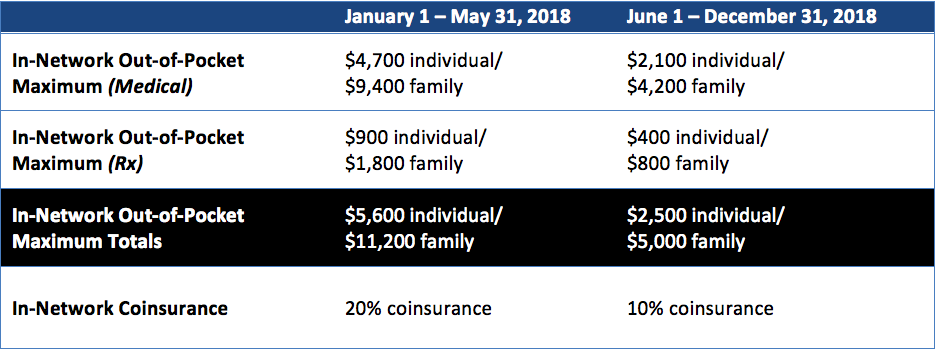
Plan Option A (PPO): Reduced In-Network Out-of-Pocket Maximums & Coinsurance
Effective June 1, 2018, the amounts for in-network coinsurance and out-of-pocket maximums will be reduced by 50% or more. See the chart below for details on the upcoming changes. If you wish to remain in Plan A, no action is required on your part and the plan changes below will become effective June 1, 2018.
Plan Option B (PPO): No Changes to Plan Option B
There are no changes to the PPO Plan Option B as a result of the new plan change. If you wish to move from Plan Option B to Plan Options A or C, you must complete the Special Benefits Enrollment form enclosed in this packet.
Plan Option C (Kaiser Permanente®): Reduced Out-of-Pocket Maximums & Coinsurance
Effective June 1, 2018, the amounts for coinsurance and out-of-pocket maximums will be reduced by 50%. See the chart below for details on the upcoming changes. If you wish to remain in Plan C, no action is required on your part and the plan changes below will become effective June 1, 2018.
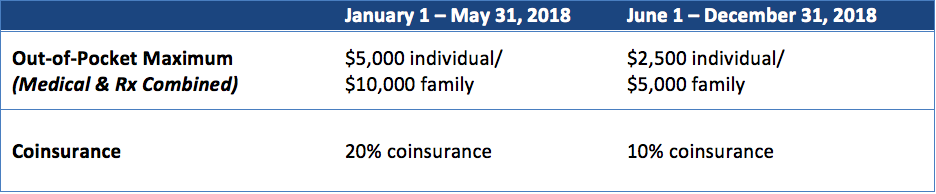
Understanding the Mid-Year Changes to the Out-of-Pocket Maximums
Given that the changes to out-of-pocket maximums will occur during the plan year, it’s important to understand how the changes may affect your wallet. For starters, if you reach the out-of-pocket maximum for the period between January 1 – May 31, 2018, then you will not have any additional out-of-pocket costs for the remainder of the 2018 plan year. Additionally, if during that same period you have already reached the out-of-pocket maximum amount for the period after June 1, 2018, then you will not have any additional out-of-pocket costs for the remainder of the 2018 plan year.
However if by June 1, 2018, you have not reached the out-of-pocket maximum for the remainder of the plan year (e.g. $2,500 individual or $5,000 family), then you will be responsible for any charges up to the new maximum amounts for the remainder of the 2018 plan year. For example, if you have spent $2,000 by June 1, 2018 as an individual, then you will be responsible for no more than $500 of out-of-pocket expenses for the remainder of the 2018 plan year.
As a reminder, the out-of-pocket maximum applied is based on the date of service and the benefits available at the respective date of service. It is not based on the date the claim is received.
Special Note for Current Section 125 Plan Participants
If you are currently deducting medical premiums on a pre-tax basis and will be switching plan carriers (i.e. switch from Plan Option A/B to Plan Option C or vice versa), you will need to contact American Fidelity Assurance Company (AFA) by no later than June 30, 2018 to complete a new election form. Failure to do so will result in your new medical plan carrier premiums to be deducted on a post-tax basis. For more details, please contact AFA:
- American Fidelity Assurance Company (AFA)
Central California Branch Office
3649 W. Beechwood Ave., Suite 103
Fresno, CA 93711
Toll-free: 866-504-0010, Extension 0
Local: 559-230-2107, Extension 0
www.americanfidelity.com
NOTE: Health Care Flexible Spending Account and Dependent Care Flexible Spending Account changes are not allowed during this Special Benefits Enrollment.
Review the Enrollment Packet Materials
In the coming days, eligible plan participants will receive the full special benefits enrollment packet at their homes with detailed information and the required forms. Until then, you may download and review the following forms to complete the Special Benefits Enrollment:
- Active Employee – Special Benefits Enrollment Forms
- COBRA Participant – Special Benefits Enrollment Forms
- EdCode Participant – Special Benefits Enrollment Forms
- Medicare-eligible Retiree – Special Benefits Enrollment Forms
For additional plan information and/or provider contact information visit: www.JHMBHealthConnect.com/your-benefits.









